More than nine out of every 10 patients who survive a prescription-opioid overdose are able to get the drugs again, usually from the same prescriber, according to a study published Tuesday that underscores the uphill battle that state and federal leaders face in fighting a national drug epidemic.
By combing through insurance claims, researchers found that 91 percent of the 2,848 patients they studied continued to be prescribed the drugs, even though prescribing guidelines say overdoses and other adverse event offer “compelling reasons to withdraw prescription opioids,” Dr. Jessica Gregg wrote in an editorial that accompanies the study in the Annals of Internal Medicine.
Dr. Gregg says the authors’ findings reflect blind spots in the system, rather than slipshod prescribing, in that many of the doctors or other prescribers probably did not know that their patients had overdosed.
“There are currently no widespread systems in place, either within health plans or through government organizations for notifying providers when overdoses occur,” she wrote. “Until such systems exist, providers will be left to act with dangerously limited knowledge.”
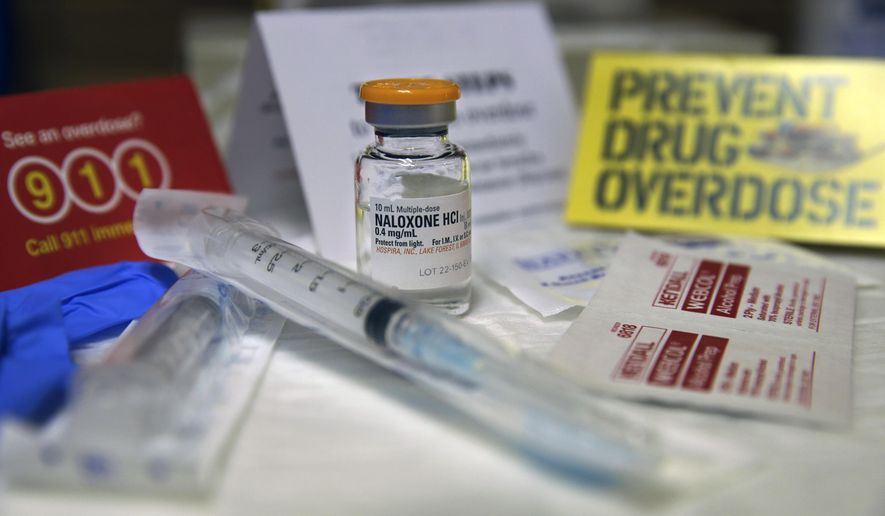
State and federal policymakers have been scrambling to deal with widespread abuse of opioid painkillers such as oxycodone, hydrocodone and hydromorphone.
Opioid drugs affect the body in a similar way to heroin, though they’re usually artificial compounds rather than derivatives of the opium poppy.
SEE ALSO: Planned Parenthood’s patients, services drop as its federal funding jumps: report
Earlier this month, the Centers for Disease Control said the rate of opioid overdose deaths from prescription drugs and heroin hit record levels in 2014 — from 7.9 per 100,000 people in 2013 to 9.0 per 100,000 in 2014, an “alarming” 14 percent increase.
The scourge has gripped wide swaths of the country, particularly in rural areas, and more than half of all Americans say they or someone they know has abused prescription painkillers, according to a recent Kaiser Family Foundation survey.
Health and Human Services Secretary Sylvia Mathews Burwell has singled out painkiller abuse as a bipartisan issue that must be addressed, and Congress used an end-of-year spending bill to boost funding for opioid-abuse prevention to $123 million, or nearly three times last year’s levels.
New Jersey Gov. Chris Christie injected the issue into the 2016 race for the GOP presidential nomination, saying it’s time to treat addicts as people who need help and not as bad apples who somehow got what was coming to them.
For now, researchers said existing state prescription monitoring programs should be reformed so that they consistently alert doctors to overdoses. Then, prescribers armed with the information should be taught how to taper off medication or use detoxification drugs such as buprenorphine.
Dr. Gregg wrote that it is often difficult for doctors to handle the overlap between pain management the risk of addiction, due to little training or resources. Also, doctors may be reluctant to draw down medication if patients insist it is the only thing that manages their pain and helps them get out of bed in the morning and tend to their families.
SEE ALSO: Bacon ‘desecration’ puts Las Vegas mosque at center of anti-Muslim hate crime probe
Others may believe that stopping prescription opioid treatment will lead patients to seek illegal alternatives, namely heroin.
Researchers did find a silver lining in the results. Doctors tended to prescribe opioids at lower dosages after an overdose compared to the 90 days leading up to the event, suggesting some providers were actually aware of what happened, or that patients asked for less of the drug.
“Either way, something changed,” Dr. Gregg wrote. “The overdose event was a potentially pivotal moment for patients and physicians, a moment when intervention might be possible and welcome.”
• Tom Howell Jr. can be reached at thowell@washingtontimes.com.



Please read our comment policy before commenting.